Carers of Elderly Persons and Working Age Persons with Sickness, Injury and Disablement
ISE02/2023

- Concern regarding heavy practical demand and mental burden on carers (or "caregivers") in the community often heightens following tragedies related to carers harming their dependants as they reckoned that their caring responsibilities have become unbearable. Legislative Council ("LegCo") Members have repeatedly pressed the Government to provide pragmatic relief to carers. On 30 November 2022, LegCo passed a motion on "Implementing 'Carer-centric' Policy" to urge the Government to provide more comprehensive financial, psychological, social life, care knowledge and resource matching support to carers1Legend symbol denoting Back on 2 June 2021, LegCo also passed another motion on "Enhancing Support for Carers," urging the Government to step up allowance schemes, set up a comprehensive carer support framework, increase emergency respite places, and establish a carer database etc.; recently at a committee meeting held on 13 February 2023, members of the LegCo Panel on Welfare Services supported the proposal to appoint a subcommittee for studying policy issues related to carers in the community.
- This issue of Essentials will attempt to provide broad observations related to the socio-economic and other characteristics of the carers population in Hong Kong (focusing on carers of (a) elderly persons, i.e. aged 65 and above, and (b) working age persons (i.e. aged 15-64) with sickness/injury/disablement2Legend symbol denoting It must be acknowledged that caring responsibilities for children (i.e. persons under 15 years old) is another key component in the carers community. In particular, the additional challenges faced by carers of children with disabilities and/or chronic diseases should not be ignored. However, child caring and child rearing are complex issues spanning family, social services, labour market and population policies, among other things. It is therefore beyond the narrower scope of this Essential which focuses on carers of persons in other age groups.) as well as Government policies to support carers and stakeholders' views on the relevant policies. Experience in Australia related to carer support will also be discussed.
Carers in the local community
- There is no international consensus on exact definition of carers. Making reference to organizations including International Alliance of Carer Organizations and Carers Alliance Hong Kong as well as relevant government authorities around the world:
-
(a)carers include people who provide help and care to another person to satisfy the person's various practical demands in day-to-day living and support mental wellbeing arising from diminishing physical ability, a debilitating cognitive condition or a chronic life-limiting illness;
-
(b)care can be provided in the format of either formal care (usually performed by paid employees of hospital, healthcare providers and social services organizations, as well as domestic helpers) or informal care (usually on an unpaid basis); and
-
(c)for informal carers specifically, they broadly include family members, relatives and friends (though some commentators may also include neighbours or other significant individuals) who take on a caring role to offer support to someone with practical and mental wellbeing needs as mentioned at (a).
-
- From desktop research, there appears no publicly available statistics so far to provide a comprehensive overview on the number of informal carers in Hong Kong and their profile. Nevertheless, several sets of statistics and reports from the Census and Statistics Department, including data compiled from the 2019-2020 Supplementary Enquiries on Persons with Disabilities and Chronic Diseases (and their Carers) ("Supplementary Enquiries3Legend symbol denoting The Census and Statistics Department ("C&SD") conducts supplementary enquiries attached to the regular General Household Surveys on an ad hoc basis. A territory wide survey on persons with disabilities and chronic diseases was conducted during August 2019 to December 2020 to estimate the total number and prevalence rate of persons with selected types of disabilities and chronic diseases, together with information about the carers of these persons. According to C&SD, the data intends to reflect the situation in 2020. See Census and Statistics Department (2021)."), statistics from the 5-yearly Population Census/By-census, and the recently published 2021 Population Census Thematic Report: Older Persons ("Thematic Report"), can all shed light on population of care recipients4Legend symbol denoting The data on care recipients discussed in this Essentials refers to care recipients who resided at home (or resided in households). Persons residing in institutions and special classes buildings, meanwhile, are not included. and their carers' characteristics5Legend symbol denoting Much of the data discussed in the ensuing paragraphs are provided by C&SD upon request by the Research Office. .
- More specifically in the above-mentioned Thematic Report, a chapter was dedicated to statistics covering older long-term care recipients (i.e. aged 60 and above)6Legend symbol denoting Older long-term care recipients are defined as "persons aged 60 and above who currently need relative(s) or other person(s) to take care of their day-to-day living (such as domestic activities, going shopping, going to recreational centre, consulting doctors and taking medicine/receiving treatment) on a long-term basis". See Census and Statistics Department (2023). as well as that for their primary carers (i.e. the carer who provided the longest hours of caring services during a week). According to the Report, around 226 000 older long-term care recipients had spouses, sons/daughters or sons-in-law/daughters-in-law acting as their primary carers7Legend symbol denoting Among these 226 000 older long-term care recipients, 179 000 (i.e. 79%) of them lived together with their primary carers while the remaining 46 000 (21%) were not living together with their primary carers. For the other 95 000 older long-term care recipients (i.e. their primary carers were not their spouses, sons/daughters or sons-in-law/daughters-in-law), around 68 000 and 6 000 had live-in domestic helpers and staff from social welfare organizations as their primary carers respectively; the remnant, around 20 000 care recipients, had other persons (including relatives other than spouses, sons/daughters or sons-in-law/daughters-in-law, and friends) acting as their primary carers. Separately, given primary carers might take care of one or more than one older long-term care recipients, the number of primary carers would likely be lower than the corresponding number of care recipients. Using data from the Thematic Report as an illustration, among cases where the older long-term care recipients lived together with their primary carers, there were 234 000 primary carers responsible for supporting 257 000 older long-term care recipients, i.e. a differential of close to 10%. See Census and Statistics Department (2023). in 2021.
- Regarding the Supplementary Enquiries, it provided data specifically on care recipients with disabilities and/or chronic diseases8Legend symbol denoting Care recipients with disabilities and/or chronic diseases are defined as persons with specific needs (i.e. persons who were encountering difficulty in day-to-day living due to disabilities and chronic diseases, and persons with chronic diseases who were using assistive devices) and had another person taking care of their day-to-day living. For details on definition of persons with disabilities and persons with chronic diseases in the Supplementary Enquiries, see Census and Statistics Department (2021). (including the number of care recipients with selected characteristics9Legend symbol denoting From the Supplementary Enquiries' data provided by C&SD upon request, it can be observed that, in 2020, there were about 36 000 to 69 000 working age care recipients with disabilities and/or chronic diseases receiving day-to-day care from their family/relatives/friends. However, it is difficult to pin-point a more precise figure – there could be duplication between the two sets of data on persons with disabilities and persons with chronic diseases respectively (as a person may suffer from disabilities and chronic diseases at the same time), but ascertaining the degree of duplication is not feasible as the two sets of data were collected from two separate surveys which were conducted over different data collection periods. The figure arising from simply adding the two sets of data directly, therefore, can only be considered an "upper bound" estimate of care recipients. For more detailed data on regarding the caring need and arrangement for persons with disabilities and/or chronic diseases, see Appendix 1.), covering not only elderly care recipients but those in other age groups as well. By further focusing on care recipients with family/relatives/friends (who are usually considered informal carers)10Legend symbol denoting Family/relatives include, for example, spouses, parents, children, sons-in-law, daughters-in-law and siblings. Although some commentators consider neighbours as a category of informal carers, this Essentials puts its focus on the roles of family, relatives and friends as carers, thus neighbours are excluded from all data herein. acting as their sole carers or primary carers, selected characteristics of their carers are set out in the table below:Figure 1 – Care recipients(1) by age and whether had disabilities/chronic diseases: selected characteristics of their carers
Sole or primary carers(2): share (%) of selected characteristics Age: 65 and above Gender: Female Had a job Elderly (aged 65 and above) care recipients With disabilities 35 65 38 With chronic diseases 42 65 33 Working age (aged 15-64) care recipients With disabilities 1411Legend symbol denoting The ratios of relevant carers reported to be aged 35-54 and aged 55-64 were 43% and 31% respectively. 65 41 With chronic diseases 1512Legend symbol denoting The ratios of relevant carers reported to be aged 35-54 and aged 55-64 were 27% and close to 40% respectively. 55 38 Notes: (1) See Endnote 8 for definition of care recipients. Data in the table covers care recipients who were economically inactive13Legend symbol denoting The economically inactive population is made up of those persons who have not had a job and have not been at work during the 7 days before enumeration (excluding persons who have been on leave/holiday during the period and unemployed persons during the 7 days) as well as homemakers, retirees, unpaid carers, persons who are not available for work, and persons who are not seeking work. As for the economically active population (which is synonymous with the labour force), it comprises the employed population and the unemployed population..(2)Data in the table covers informal carers including family, relatives and friends, and does not include formal carers (domestic helpers, private nurses at home and nursing staff).Source: Census and Statistics Department. - From the data above, it can be observed that:
-
(a)the oft-discussed cases of elderly persons being taken care of by other elderly persons are not uncommon — among the elderly care recipients with disabilities and/or chronic diseases as covered by the table above, about 40% reported having family/relatives/friends aged 65 and above as their sole or primary carers;
-
(b)on the other hand, among working age care recipients with family/relatives/friends as their sole or primary carers, less than 20% of their carers were elderly persons; and
-
(c)regarding gender and employment status of carers, for sole or primary carers who were responsible for taking care of family/relatives/friends, two-thirds were female (though the ratio was somewhat lower for working age care recipients with chronic diseases) while a noticeable share had a job as well (ranging from 33% to 41%).
-
- Data on older persons and "unpaid carers14Legend symbol denoting It should be cautioned that the category of unpaid carers depends on self-identification by the respondents. This option, meanwhile, fails to capture carers who are (a) economically inactive and self-identify as other categories such as homemakers, retirees and, for young carers in particular, students; and (b) economically active (i.e. carers participating in the labour market). Besides, the data cannot distinguish the intensity of caregiving responsibilities of carers. While some are heavily involved in caring for day-to-day living of another person (e.g. they act as the primary carers), there are other carers who only provide ad hoc and less intensive caregiving. Hence, the data covers both sole/primary carers and persons with other caregiving responsibilities, and therefore cannot be compared directly with the data on carers obtained from the Supplementary Enquiries and that on carers of older persons from the 2021 Population Census." from 2021 Population Census also echoes, to a certain degree, the observations above arising from the Supplementary Enquiries:
-
(a)for spouses, sons/daughters or sons-in-law/daughters-in-law who acted as primary carers and lived in the same accommodation with their older long-term care recipients, 39% of these carers were aged 60 and above themselves, thereby reflecting the prevalent situation of elderly persons being taken care of by other elderly persons15Legend symbol denoting The figure does not include live-in domestic helpers, staff of social welfare organizations (e.g. day care centre services, home-based care services) and "others" (relatives other than spouses, sons/daughters or sons-in-law/daughters-in-law, and friends etc.). The Thematic Report pointed out that when including all formal carers (live-in domestic helpers and staff of social welfare organizations etc.) and informal carers (spouses, sons/daughters, sons-in-law/daughters-in-law, other relatives, and friends), about 29% of primary carers who lived in the same accommodation with their older long-term care recipients were aged 60 and above themselves.;
-
(b)among the 24 700 unpaid carers in households with economically inactive elderly members16Legend symbol denoting Elderly unpaid carers are excluded. but, at the same time, no children nor any economically inactive working age persons with sickness/injury/disablement, a noticeable share of 26% (6 300 persons) were themselves elderly persons17Legend symbol denoting As some unpaid carers might have been responsible for caring for persons residing in another household, the share of elderly persons in unpaid carers in these households is only for reference., 18Legend symbol denoting Another noteworthy observation is that for households with both economically inactive elderly persons and children, elderly unpaid carers accounted for a significantly lesser share of just 6% (800 persons) of the 12 800 unpaid carers in these households, whereas female aged between 35 and 54 years old made up a much more noticeable share of unpaid carers in these households, at 56% (7 100). In fact, among over 160 000 persons who identified themselves as unpaid carers in the 2021 Population Census, the biggest group, at 56% or 90 800 persons, were actually found in households with caring responsibilities likely confined to taking care of children (i.e. households with children but no persons who are economically inactive elderly persons or are working age persons who are economically inactive due to sickness/injury/disablement).; and
-
(c)another 5 400 unpaid carers (3% of all unpaid carers) were in households with economically inactive working age persons with sickness/injury/disablement — elderly persons (include both genders) accounted for one-eighth of unpaid carers in these households, whereas female aged 35-54 and female aged 55-64 had higher shares (each group took up roughly a quarter of the unpaid carers in these households).
-
Government support for informal carers of elderly persons and of persons with disabilities
- The Government acknowledges that family/relatives/friends serving as informal carers play an important role in supporting elderly persons and persons with disabilities to live in the community. With a view to enhancing carers' caring capability and relieving their pressure, the Government provides a number of financial assistance programmes for carers and a range of subvented services in support of carers, including centre-based services (e.g. care skills training, counselling, emotional support), home-based services (e.g. personal care, home cleaning, rehabilitation training) and respite services, etc. (details are at Appendix 2).
- Financial support: The Government announced to regularize three schemes, namely, Living Allowance for Carers of Elderly Persons from Low-income Families, Living Allowance for Low-income Carers of Persons with Disabilities, and Special Care Subsidy for the Severely Disabled. Furthermore, the monthly living allowance for carers from low-income families will be increased by 25% from $2,400 to $3,000, benefitting about 10 000 carers, while the monthly full grant of the Special Care Subsidy for the Severely Disabled will increase from $2,000 to $2,500 as well. Various financial assistance under the existing system, including disability allowances and tax allowances, can offer financial relief to carers as well.
- Centre-based community care and support services: Over 300 centres/units provide services to elderly persons, including meal services, provision of information on resources and services, and carer support services; for persons with disabilities, over 60 centres in various forms offer a wide range of assistance ranging from training and capacity building for both the persons with disabilities and their carers to emotional support, counselling services, and support networks. Another 245 service places are offered in the Care and Attention Homes for Severely Disabled Persons, District Support Centres for Persons with Disabilities ("DSCs"), and Community Rehabilitation Day Centres. Such support services can help alleviate carers from the pressure of taking care of their family/relatives/friends for prolonged periods.
- Home-based community care and support services: For elderly persons, around 13 000 service places are provided (services include personal/basic/special care, housekeeping and meal delivery services, carer support, etc.); for persons with disabilities, 6 service teams of Home Care Service for Persons with Severe Disabilities and 2 service teams of Integrated Support Service for Persons with Severe Physical Disabilities are responsible to provide various types of support. Similar to centre-based support, the relevant services can also lessen burden on carers arising from taking care of day-to-day living of another person.
- Respite services: Close to 600 designated respite places are provided for elderly persons through subvented Residential Care Homes for Elderly and contract homes, private homes participating in the Enhanced Bought Place Scheme, and subsidized Day Care Centres/Units for the Elderly. The number of respite places offered is similar for persons with disabilities, through a wide variety of centres including Day Activity Centres, DSCs, Care and Attention Homes for Severely Disabled Persons, and Residential Care Homes for Persons with Disabilities.
- Other support: Social Welfare Department ("SWD") offers hotline service and webpages to publicize information on welfare services and information on relevant carer support services. SWD will commission a non-governmental organization ("NGO") to set up a designated 24-hour hotline for carers in the third quarter of this year to provide instant consultation and counselling, outreaching, emergency support and referral services and launch a one-stop information gateway towards end-2023. Project-based services also provide support for discharged elderly patients, elderly persons with dementia, as well as their carers.
Stakeholders views on existing Government policies
- There is a general understanding in the community that informal carers have been selflessly devoting years and years of their lives to relieve the burden on and make great contribution to society, and it is therefore generally agreed that the Government should strengthen the "carer-centric" principle in formulating policies and define carers as "priority service users". However, there are views that given the lack of long-term planning for elderly and rehabilitation care services in Hong Kong, users may need to wait for a number of years before being provided with care services (including residential care). As a result, carers need to discharge their caring responsibilities for extended periods, putting them under prolonged financial, physical and psychological stress, especially in the case of working carers who may not be entitled to flexible work and leave arrangements that suit their status as carers. Apart from financial assistance, there are also views emphasizing the importance of community care and support services, caring skills training, and mental and psychological support to carers.
- Commentators also raised a number of concerns including (a) the absence of a clear definition of carers; (b) reliance on carers to hunt for support services, leading to high search cost, service mismatch and ever low utilization rate for certain services; and (c) the lack of comprehensive and personalized support for carers (especially on their physical and mental wellbeing). The ensuing paragraphs will discuss these issues in more details.
- So far, the Government has neither formally established methodology in identifying carers nor set out a standardized and clear definition of carers at the policy level19Legend symbol denoting Earlier, the Government released a consultancy report, mentioning the situations of carers of elderly persons and persons with disabilities. However, the no concrete definition on carers was put forward. See PolyU Consultancy and Technology Co Ltd (2022)., 20Legend symbol denoting In relation to a systematic "professional carer system" comprising a tripartite partnership among the Government, professional care providers and carers, it is proposed that professional care providers adopt a case management model to assess the needs for care and attention of the care recipients, enter into a service agreement with the carers to regulate their obligations, and at the same time, provide them with training on proper caring skills. Once a service agreement has been entered into, it is like being accredited by the Government as the carers' social status has been established. See Legislative Council Secretariat (2022).. Many experts in the fields of carer and welfare research thus opine that the absence of a clear definition may have contributed to the fact that data collection and analysis on carers conducted by the Government and in the community are often fragmented and on an one-off basis. This has not only failed to support more comprehensive and in-depth analysis, but also made it difficult to conduct meaningful observations on how the circumstances and needs of carers have evolved in the past years.
- Moreover, stakeholders consider support services for carers and care recipients in Hong Kong as rather fragmented, rendering it difficult for those in need to seek suitable services, particularly when carers may not be able to immediately find the service they need in unexpected circumstances. It is therefore necessary to consider, for example, setting up one-stop support service centres in all 18 districts in Hong Kong to better align demand and supply.
- Meanwhile, partly owing to the difficulty faced by carers and care recipients in search for suitable services, centre-based services are in short supply overall on the one hand while the utilization rate of certain services remained low on the other hand (for instance, the utilization rate of designated day respite services for elderly persons was only between 40% and 50% in 2019-2020 according to some statistics21Legend symbol denoting To facilitate the public's checking of the vacancies of residential respite places which suit their needs, the Social Welfare Department ("SWD") launched the online "Vacancy Enquiry System for Residential Respite Service for Persons with Disabilities, Residential Respite Service for the Elderly and Emergency Placement for the Elderly" in 2019. SWD plans to enhance the Enquiry System in mid-2023 to cover day respite services, and assist carers' simultaneous search for day and residential respite services through the System. See GovHK (2022c).). In particular, given the suspension of community care services amid the COVID-19 epidemic over the past three years, quite a number of members of grass-roots families need to break from regular employment and take care of mobility-handicapped or chronically ill elderly persons and family members at home, thus worsening the financial situation of their families and increasing their pressure.
- Many studies on carers further indicate that carers may not understand their own physical and psychological state, making it difficult for early identification of the problems they may face in daily life and seek appropriate support, thereby considered another worrying phenomenon. In fact, different studies have noted that carers fare worse than non-carers in various domains of quality of life, including requiring more doctor visits, prevalence of anxiety and depression and a higher chance of weight loss. As this may be closely related to generally longer hours of caring services provided by carers in Hong Kong, there is a strong demand among carers for "short breaks" (ranging from elder sitting or home help services and respite services to "enjoy breaks outside homes", hotline services and support groups).
- Other issues raised include carers not necessarily having the right knowledge of care, making use of technology to help ease the burden of carers, concerns about "seniors caring for seniors" and "seniors and persons with disabilities caring for each other", and carers of chronically ill patients not necessarily benefiting from support measures for carers of the elderly/disabled persons22Legend symbol denoting There are criticisms that the threshold is not low for a chronically ill patient to be considered as severely disabled within the meaning of the Social Security Allowance Scheme. Specifically, the applicant must be certified by the Director of Health or the Chief Executive, Hospital Authority (or under exceptional circumstances by a registered medical practitioner of a private hospital) as falling into one of the following categories: (a) illness resulting in being bedridden; (b) a degree of disablement resulting in the applicant needing substantial help from others to cope with daily life (i.e. significant restriction or lack of ability or volition to perform at least one or more of the following activities in daily living to the extent that substantial help from others is required: (i) working in the original occupation and performing any other kind of work for which he/she is suited; (ii) coping with self-care and personal hygiene such as feeding, dressing, grooming, toileting and/or bathing; (iii) maintaining one's posture and dynamic balance while standing or sitting, for daily activities, managing indoor transfer (bed/chair, floor/chair, toilet transfer), travelling to clinic, school, place of work; or (iv) expressing oneself, communicating and interacting with others, maintaining cognitive abilities (orientation, attention, concentration, memory, judgment, thinking, learning ability, etc.), maintaining emotional control and social behaviour). See 1823.gov.hk (2021)., etc.
- The Labour and Welfare Bureau commissioned The Hong Kong Polytechnic University Consulting Team in July 2020 to conduct a consultancy study on the needs of and support required by informal unpaid carers of elderly persons and persons with disabilities in Hong Kong. The Consultant presented the final report to the Government in June 2022 and proposed the Triple S Model (or three "gears"), namely (a) carer strength building; (b) encouraging family and informal support; and (c) service integration. Under this model, 11 specific recommendations were put forward, including developing a carer-centric information gateway, strengthening carers' ability, cultivating a carer-friendly neighbourhood and support environment in the workplace, identifying high-risk carers and providing timely support, and increasing respite service23Legend symbol denoting The 11 recommendations are: Gear I: Carer Strength Building (a) Raise awareness of carers about the importance, availability, and access of information and increase the readiness of carers and intermediate parties to seek help from available services; (b) Examine existing websites and encourage non-governmental organizations/social enterprises/corporates to develop a carer-centric and sustainable information gateway to address carers' needs; (c) Provide carer-centric training and intervention to promote carers' wellbeing, self management, ability to cope with stress, as well as to strengthen their caregiving capacity; Gear II: Encouraging Family and Informal Support (d) Promote family-based support and mutual assistance among peer carers across their lifespan and at different stages of their caregiving journey; (e) Cultivate a carer-friendly neighbourhood; (f) Devise and promote a carer-friendly support environment in the workplace so as to help carers strike a balance between their work and their caregiving role; Gear III: Service Integration (g) Develop a local self-administered assessment tool with the aim of increasing the knowledge of carers in terms of needs, risks identification and management, and potential support available; (h) Identify high-risk carers and provide timely support; (i) Better introduce, access and utilize assistive technologies to relieve care burden, enhance caring capability and improve carers' quality of life; (j) Increase accessibility and diversity of respite service to provide relief to carers with ad-hoc needs; and (k) Provide good mix of services, voucher and cash to support carers. See PolyU Consultancy and Technology Co Ltd (2022).. The Government agreed in principle to the recommendations of the consultancy study and briefed members of the LegCo Panel on Welfare Services on the recommendations at its meeting in July 2022.
Legal definition of carers
- The Australian Government passed the Carer Recognition Act ("the Act") in 201025Legend symbol denoting In May 2009, Australian House of Representatives Family, Community, Housing and Youth Committee published a report entitled "Who Cares ...?". Apart from urging for "immediate financial relief" for carers, the report also advocated for greater access to respite services (as a "time-out" for carers from their caring roles), better coordination of support services, setting up a one-stop shop for information on community care services, establishing nationally consistent and streamlined support systems, promulgating a national carer recognition legislation, and improving training and support to carers in employment. See Standing Committee on Family, Community, Housing and Youth, House of Representatives (2009a, 2009b)., 26Legend symbol denoting Each of the six states and two territories in Australia have carer laws and/or policies. See Carer Gateway (undated). to increase recognition and awareness of informal carers and to acknowledge the valuable contribution they make to the wider society. The Act provides a nationwide legal definition of a "carer," as an individual who provides personal care, support and assistance to another individual who needs them because that other individual (a) has a disability; (b) has a medical condition (including a terminal or chronic illness); (c) has a mental illness; or (d) is frail and aged. The Act, meanwhile, excludes people who provide care (a) under a contract of service or a contract for the provision of services; (b) in the course of doing voluntary work for a charitable, welfare or community organization; or (c) as part of the requirements of a course of education or training.
- Although the Act does not create legally enforceable rights or duties, it provides a statement of 10 principles as to how carers should be treated, so that, among other things, (a) all carers should have the same rights, choices and opportunities (including employment and education) as other Australians; (b) their valuable social and economic contribution to society should be recognized and supported; and (c) they are acknowledged as individuals with their own needs within and beyond their caring roles.
- According to the Australian Bureau of Statistics Survey of Disability, Ageing and Carers, 2.65 million people (or roughly 10.8% Australians) provided informal care in Australia in 201827Legend symbol denoting The relevant figure was 11.6% in 2015. See Australian Bureau of Statistics (2019).. More specifically:
-
(a)around 1 in 3 carers (33% or 862 000 people) were primary carers, meaning they provided the most care to the person needing support in one or more core activities (self-care, mobility and communication); the other carers were considered "other informal carers" who provided informal care to someone but were not their primary carer;
-
(b)primary carers were most commonly female (72%, compared with 50% of other carers);
-
(c)the age group of 55 to 64 years old had the highest proportion in providing informal care, at close to 20% (ratios for male and female in this age group were 16% and 23% respectively);
-
(d)the number of primary carers aged 55-64 was 206 000 (149 000 were female), followed closely by those aged 45-54 at 198 000 (148 000 were female); and
-
(e)it further noted that 37% of primary carers had disabilities28Legend symbol denoting Defined as having any limitation, restriction or impairment which restricts everyday activities and has lasted, or is likely to last, for at least six months. See Australian Bureau of Statistics (2019)., a much higher ratio than non-carers (15%).
-
Financial support
- In terms of financial support, the means-tested Carer Payment provides income support for carers caring for someone who has considerable needs due to disabilities or ill health, making them unable to support themselves through substantial paid employment. As at September 2022, 302 000 people received Carer Payment29Legend symbol denoting Of people receiving the Carer Payment at September 2022, 80% were being paid the full rate of payment (meaning their assets and income were both below relevant thresholds) and almost half (49%) had been receiving the payment for 5 years or more. See Australian Government (2022).. For 2022-23, A$7.1 billion (HK$38.9 billion) was budgeted for such payments30Legend symbol denoting See Department of Social Services (2022b)..
- People may also, or instead, receive the Carer Allowance, which is a smaller supplementary payment for carers who provide daily care and attention at home for a person with a disability, severe medical condition or who is frail and aged. The Carer Allowance may be paid in addition to income support payments. At September 2022, 626 000 people received this allowance31Legend symbol denoting See Australian Institute of Health and Welfare (2021a)., and A$2.6 billion (HK$14.2 billion) has been allocated in 2022-23 for such payments32Legend symbol denoting See Department of Social Services (2022b)..
- It is noted that two other programmes further cater to support specific groups of carers:
-
(a)Carer Adjustment Payment will provide one-time ex-gratia payment of up to A$10,000 (HK$55,000) to families in exceptional circumstances who do not qualify for any government income support payments and who experience a catastrophic event where a child under 7 years old is diagnosed with a severe disability or severe medical condition33Legend symbol denoting A$2.8 million (HK$15 million) was allocated for 2022-23. See Department of Social Services (2022b).; and
-
(b)Young Carer Bursary Program supports young carers aged 12-25 to continue with their education, offering 1 000 bursaries of A$3,000 (HK$16,000) each year34Legend symbol denoting The programme was introduced in 2020 as a 3-year pilot scheme, though Internet search indicates that the programme is still on-going with applications accepted during July to September each year. The Department of Social Services requires all successful Young Carer Bursary applicants to complete a mandatory survey in May and October each year to assess their ongoing eligibility. Recipients will be considered ineligible if they are no longer studying (including deference and leave of absence), receive another bursary or scholarship, do not complete surveys and/or have ended their caring roles. Recipients will receive A$2,000 (HK$11,000) at the start of the year, and then receive a second payment of A$1,000 (HK$5,500) in June after completing the mid-year survey in May. They can use the funding towards education or training, including but not limited to school fees, laptops and software, uniforms, transport and accommodation, respite care, emotional support, and extracurricular activities. See Department of Social Services (2020) and Young Carer Network (undated-a, undated-b, undated-c).. Recipients can also become part of a network to access helpful resources by sharing their experience and tips with other young carers on dealing with some common situations.
-
Integrated approach to provide support and advice
- The Carer Gateway, launched in 2015, serves as a digital and telephone-based platform to provide information on community care and support services. Each region in Australia has a Carer Gateway Service Provider, who can talk through what carers need and help them find local services and support. In addition, the Carer Gateway offers phone counselling, on-line carer forums to allow carers to connect with others, online self-guided coaching and online skills courses. After an extensive four-year consultation process with carers and the professional care sector, the delivery of in-person services was also introduced in April 2020. The Australian Government committed A$33.7 million (HK$185 million) over the initial 4 years of the project, and subsequently provided additional funding of A$700 million (HK$3.8 billion) and A$103 million (HK$560 million) later to Carer Gateway with a view to improving the pathways available to informal carers when accessing support services.
- Moreover, the Australian Government put much emphasis on developing the Integrated Carer Support Service ("ICSS") model to help carers early in their caring role, increase their skills and reduce the strain of caring. While typical centre-based and home-based community care and support services are also being offered (more details in the ensuing paragraphs), the ICSS Service pathways35Legend symbol denoting See Department of Social Services (2018). distinguish themselves by including a "Carer Support Planning" process performed by Carer Gateway Regional Delivery Partners ("RDPs") generally in the early stage of engagement with carers, usually right after the carers' entry into the pathways (i.e. access to the services via phone, online and in-person with a RDP)36Legend symbol denoting One exception would be when carers request for emergency respite care. In such case "emergency procedures" will be triggered immediately and emergency respite services will be secured for the carers first. Carers support planning will be undertaken in follow up contacts. For carers who access services online, they could request a call-back by Regional Delivery Partners ("RDP") or get referred to RDP to follow the Carer Support Planning Process, in addition to browsing the information on the Carer Gateway website and determining the most appropriate resources on their own. See Department of Social Services (2018).. The RDP will take steps to understand carer needs, determine the services that would best suit their situation, and formulate a personalized Action Plan. The goal is to devise tailored support packages designed to provide carers with services and support specific to their needs to help carers in their caring role.
Care services programmes
- For elderly persons in Australia, Home Care Packages ("HCP") are one of the ways to access affordable care services to get some help at home, thereby alleviating the pressure on their carers. Depending on the level of HCP assistance, they can cover a range of different services including bathing, hygiene, and grooming, nursing and therapies, meals and food preparation, home chores (cleaning, laundry etc.), mobility, and social outings. HCPs are designed to be flexible and directly linked to the identified care needs and goals, and facilitate elderly persons to live safely and independently in their homes. The HCPs are co-funded by the Government37Legend symbol denoting Subsidies depend on the level of care provided in the Home Care Packages ("HCP"). Supplemental subsidies may also be made available if certain criteria are met (dementia cases, Veterans, living in rural and remote areas etc.) and/or additional services are required (e.g. oxygen and enteral feeding). and the elderly persons receiving care. The HCP recipients are generally liable for a "basic daily fee" (up to A$11.71 per day, or HK$64); subject to their income and asset level, they may also be required to contribute an "income-tested care fee" (up to A$33.59 per day, or HK$184).
- Regarding disabled persons under 65 years old with permanent (or likely to be permanent) and significant disabilities (intellectual, physical, sensory, cognitive and psychosocial disabilities)38Legend symbol denoting At 31 December 2022, around 573 300 people were active participants in the National Disability Insurance Scheme ("NDIS"). The top 5 groups, by primary disability, were autism (35% or around 199 400 people), intellectual disability (17%/98 800), psychosocial disability (10%/59 500), developmental delay (10%/56 800) and hearing impairment (4%/25 600); in terms of age profile, 51% (around 290 200 people) were aged 18 or under, 25% (142 100) were aged 19-44, and 25% (141 000) were aged 45 and above (it is noted that aged 65 and above beneficiaries accounted for 4%). See National Disability Insurance Agency (2022)., the National Disability Insurance Scheme ("NDIS")39Legend symbol denoting Budget for the NDIS in 2022-23 amounted to A$24.1 billion (HK$130 billion). See Department of Social Services (2022b). provides reasonable and necessary supports covering 15 categories including assistance with daily life, transport, assistance with social and community participation, and home modifications40Legend symbol denoting Other categories include consumables, assistive technology, coordination of supports, improved living arrangements, increased social and community participation, finding and keeping a job, improved relationships, improved health and wellbeing, improved learning, improved life choices and improved daily living.. The services provided under NDIS are positioned as supplement to other supports that disabled persons received from their informal carers as well as from mainstream/specialized services41Legend symbol denoting Examples include (a) the Information, Linkages and Capacity Building program which provides funding to deliver community projects that benefit all people with disabilities, their carers and families; and (b) Community Mental Health programs that provide assistance to people with mental illness and their families and carers to manage the impacts of mental illness on their lives and improve their overall wellbeing. and the community.
- Regarding respite services, they are offered under different programs, including42Legend symbol denoting See Australian Institute of Health and Welfare (2021a).:
-
(a)Respite services are progressively transited to NDIS — according to the last available data on services previously provided under the National Disability Agreement in 2018-19, these publicly funded services were used by 10 041 persons who had informal carers;
-
(b)The Commonwealth Home Support Programme, meanwhile, offers centre-based, cottage and flexible respite services, which were used by 17 580 persons who had informal carers in 2019-2043Legend symbol denoting Respite services account for a small component of the Commonwealth Home Support Programme ("CHSP"). The Programme is an entry-level home support program that helps older people to live independently in their homes and communities, with an aim to help people live as independently as possible through a small amount of help. Most people in the CHSP only need one or two services from the programme. See Department of Health and Aged Care (2022a).; and
-
(c)in residential aged care, respite stays of (generally) up to 63 days in a year are available, with 20 700 admissions in 2019-20 to respite care for people who were living with family members44Legend symbol denoting Representing 25% of all respite admissions; nevertheless, it should be noted that not all family members are informal carers..
-
Carer leaves
- To help carers who wish to balance between care and career obligations, the National Employment Standards establish a number of minimum entitlements for these employees in Australia, including (a) sick & carer's leave that entitles full-time employees to 10 days of paid personal leave per year (and entitles part-time employees on a pro rata basis); and (b) if taking a paid personal/carer's leave is not possible, unpaid carer's leave is available for all employees, of up to 2 days of unpaid leave each time an immediate family/household member needs care and support subject to mutual agreements between employers and employees.
Concluding remarks
- Data obtained from the Census and Statistics Department was able to identify (a) around 230 000 older care recipients who required long-term care from their family members; and (b) a few tens of thousands of working age care recipients with disabilities and/or chronic diseases who were receiving support for day-to-day living from their family/relatives/friends. Apart from pointing out the sizable population of care recipients in the community, data available also validated certain popular perceptions regarding carers, such as female carers significantly outnumbering their male counterparts, prevalence of elderly persons taking care of each other, and a noticeable share of carers having to balance between caring and work obligations. Yet the observations made in this Essentials cannot claim to be anywhere close to comprehensive.
- The Government has committed to strengthen support to the local carer community, with more resources already earmarked for the purpose of supporting the regularization of some successful pilot schemes and a number of new services in the pipeline. However, many stakeholders continued to express concern: apart from the need to play catch up for a number of formal caring services, the lack of a thorough understanding of carers' situation and specific demand means that there is risk of mismatch in demand and supply as well as fragmentation of services, or even unidentified but lingering policy gaps.
- The development of carer policies and support measures in Australia over the past decade has demonstrated certain merit of formally identifying carers for keeping track of their welfare and tailoring policy measures, especially in terms of protecting their legal rights. The one-stop shop pathway model and comprehensive action plan for individual carers appear to be promising in addressing some issues commonly raised by stakeholders, such as fragmented services, search cost and demand-supply mismatch, as well as helping the Government and RDPs in continuously monitoring the evolving situation and needs of carers. The array of measures implemented by Australia not only provide easier access to financial and practical support, "carer-centric" measures can also offer room for carers (including those in specific groups like young carers) to pursue their own aspirations and make progress in other aspects in their lives (including employment and education). Yet with only a few years of practical experience under its belt regarding these new initiatives, it may be too early to draw definite conclusion especially when the COVID-19 pandemic may have posed unique difficulty to carers and undermined the effectiveness of this nascent support system.
Caring need and arrangement for persons with disabilities and/or
chronic diseases in 2020: by age group and labour market participation
chronic diseases in 2020: by age group and labour market participation
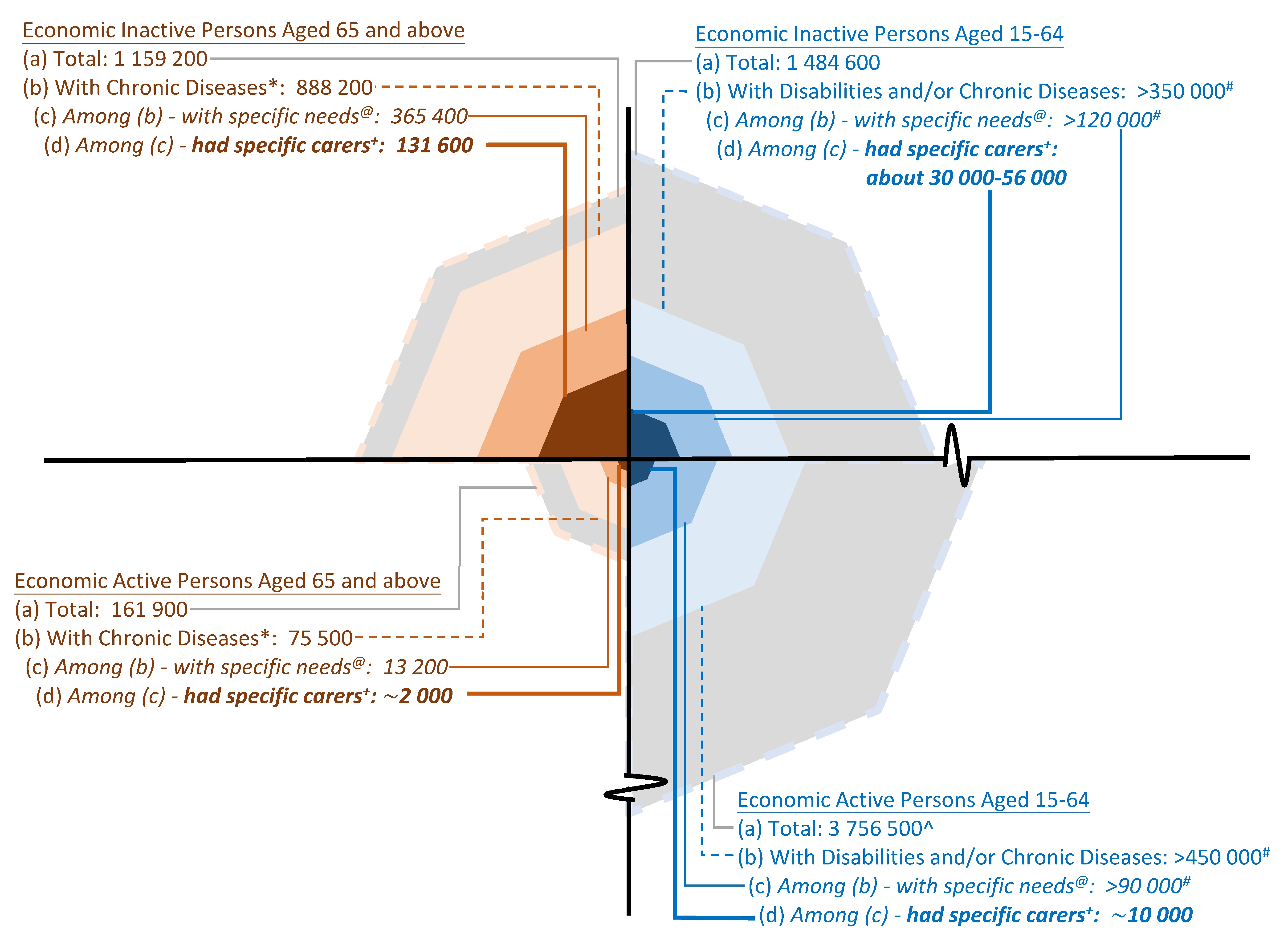
Notes: (*)In 2020, 964 000 elderly persons had chronic diseases and accounted for about 73% of elderly persons back then. To simplify the articulation, data on elderly persons with disabilities is omitted from the chart45Legend symbol denoting For reference: there were 275 600 elderly persons with disabilities; among them, 87 900 reported residing in homes and having family/relatives/friends as their sole or primary carers to take care of their day-to-day living..
(@)Defined as persons resided in households and were encountering difficulty in day-to-day living or using assistive device (for persons with chronic diseases).
(+)Specific carers are defined as family/relatives/friends acting as sole carers or primary carers to provide support to day-to-day living of another person who resided at home and had specific needs.
(#)Given it is not feasible to gauge the degree of duplication between persons with disabilities and those with chronic diseases, more concrete estimates on the number in these groups cannot be made. See Endnote 9.
(^)The number of economically active working age persons is much larger than other groups, thus the scale adopted for this group in the chart is different from that for other groups.
Sources: Census and Statistics Department, and Legislative Council Secretariat.
Caring need and arrangement for persons with disabilities and/or
chronic diseases in 2020: by age group
chronic diseases in 2020: by age group
| Age | 65 and above | 15-64 |
| Total population | 1 321 000 | 5 241 000 |
| Persons aged 65 and above and had chronic diseases |
Persons aged 15-64 and had disabilities and/or chronic diseases |
|
| Population | 964 000 | >802 000# |
| Among whom - with specific needs* | 379 000 | >200 000# |
| Among whom - had specific carers@ | 134 000 | 36 000-69 000# |
Notes: (*)Defined as persons resided in households and were encountering difficulty in day-to-day living or using assistive device (for persons with chronic diseases).
(@)Specific carers are defined as family/relatives/friends acting as sole carers or primary carers to provide support to day-to-day living of another person who resided at home and had specific needs.
(#)Given it is not feasible to gauge the degree of duplication between persons with disabilities and those with chronic diseases, more concrete estimates on the number in these groups cannot be made.
Sources:Census and Statistics Department, and Legislative Council Secretariat.
Government support for informal carers of elderly persons and
of persons with disabilities
of persons with disabilities
| Carers of elderly persons(1) | Carers of persons with disabilities(2) | |
| Financial support |
•Living Allowance for Carers of Elderly Persons from Low-income Families: initially funded by the Community Care Fund as pilots, the scheme will be regularized from October 2023 with monthly living allowance increased by 25% from $2,400 to $3,000
•The Government will also regularize the Community Care Service Voucher for the Elderly in the third quarter of 2023 (the coverage will be expanded to rental of assistive technology products as well); the number of beneficiaries will increase by 50% in phases, from 8 000 at present to 12 000 in 2025‑2026
|
•(a) Living Allowance for Low-income Carers of Persons with Disabilities and (b) Special Care Subsidy for the Severely Disabled: will also be regularized from October 2023 — for (a), monthly living allowance increased by 25% from $2,400 to $3,000; and for (b), monthly amount of full grant increased also by 25% from $2,000 to $2,500 respectively
|
| Centre-based community care and support services |
•212 District Elderly Community Centres ("DECCs") and Neighbourhood Elderly Centres provide services including educational and developmental activities, provision of information on resources and services, meal services, and carer support services (16 new Neighbourhood Elderly Centres will be set up over the next five years)
•The Support Teams for the Elderly in DECCs help identify potentially vulnerable elderly persons and their carers through outreach and community networks
•93 Day Care Centres/Units for the Elderly ("DEs/DCUs") provide services including information and counselling services, group activities and skill training, mutual support groups, and demonstration/loan of rehabilitation-aid equipment
|
•Over 60 centres, in forms of District Support Centres for Persons with Disabilities ("DSCs"), Parents/Relatives Resource Centres, Social and Recreational Centres for the Disabled, and Support Centres for Persons with Autism, offer a wide range of assistance such as training and capacity building for both the persons with disabilities and their carers; emotional support, counselling services, and support networks are also part-and-parcel to the centres' services
•245 service places are offered in the Care and Attention Homes for Severely Disabled Persons, DSCs, and Community Rehabilitation Day Centres
|
| Home-based community care and support services |
•13 365 service places are provided through Integrated Home Care Services (Frail Cases) service teams and Enhanced Home and Community Care Services service teams for elderly persons (subsidized community care services places will increase by about 300 by end-2027); services include personal/basic/special care, 24-hour emergency support, respite services, housekeeping and meal delivery services, escort services, carer support, etc.
|
•6 service teams of Home Care Service for Persons with Severe Disabilities and 2 service teams of Integrated Support Service for Persons with Severe Physical Disabilities provide a range of integrated home-based services (including personal/nursing care and rehabilitation training) for persons with disabilities in need and carer support (including counselling services, caring skills training)
|
| Respite services |
•About 570 designated respite places are provided for elderly persons through subvented Residential Care Homes for Elderly and contract homes, private homes participating in the Enhanced Bought Place Scheme, and subsidized DEs/DCUs for elderly persons
|
•About 550 respite places offered through a wide variety of centres including Day Activity Centres, DSCs, Care and Attention Homes for Severely Disabled Persons, Residential Care Homes for Persons with Disabilities
|
| Other support |
•SWD hotline service provides information on welfare services for elderly persons and persons with disabilities in the form of voice messages or facsimile transmission to callers through a 24-hour interactive voice response system, and social workers on duty also provide counselling and arrange appropriate follow-up services for those in need
•SWD will commission an NGO to set up a designated 24-hour hotline for carers in the third quarter of this year to provide instant consultation and counselling, outreaching, emergency support and referral services
•SWD websites/webpages further offer information on relevant carer support services. To provide comprehensive, updated and easily accessible information for carers of elderly persons and of persons with disabilities, SWD plans to launch a one-stop information gateway around end-2023, with an added feature to contain information on the hotline services provided by other NGOs to encourage carers to seek help whenever needed
•Project-based services also provide support for discharged elderly patients, elderly persons with dementia, as well as their carers
•To raise public awareness of the importance and needs of carers, promote mutual assistance in the community and cultivate a carer-friendly environment, SWD will, from 2023-2024, launch a three-year publicity campaign in collaboration with different stakeholders to organize a series of carer-centric programmes and public education activities
|
|
Notes: (1)The Government will expand the Hospital Authority's Integrated Discharge Support Programme for Elderly Patients in the third quarter of 2023, with the number of beneficiaries of home support services increasing from about 9 000 to 11 000.
(2)The SWD will launch a pilot scheme in the second quarter of 2023 to set up two new community rehabilitation centres for providing integrated day care and home care services for persons with severe disabilities living in the community. SWD will also regularize the Pilot Scheme on Professional Outreaching Team for Private Residential Care Homes for Persons with Disabilities from March 2023 to provide continuous multi-disciplinary professional outreach services covering social work, physiotherapy, occupational therapy and speech therapy services, etc. for about 4 000 residents of private residential care homes for persons with disabilities.
Sources: 2023-2024 Budget Speech and Labour and Welfare Bureau.
Prepared by Kent YAU
Research Office
Research and Information Division
Legislative Council Secretariat
1 March 2023
Research Office
Research and Information Division
Legislative Council Secretariat
1 March 2023
Endnotes:
- Back on 2 June 2021, LegCo also passed another motion on "Enhancing Support for Carers," urging the Government to step up allowance schemes, set up a comprehensive carer support framework, increase emergency respite places, and establish a carer database etc.
- It must be acknowledged that caring responsibilities for children (i.e. persons under 15 years old) is another key component in the carers community. In particular, the additional challenges faced by carers of children with disabilities and/or chronic diseases should not be ignored. However, child caring and child rearing are complex issues spanning family, social services, labour market and population policies, among other things. It is therefore beyond the narrower scope of this Essentials which focuses on carers of persons in other age groups.
- The Census and Statistics Department ("C&SD") conducts supplementary enquiries attached to the regular General Household Surveys on an ad hoc basis. A territory wide survey on persons with disabilities and chronic diseases was conducted during August 2019 to December 2020 to estimate the total number and prevalence rate of persons with selected types of disabilities and chronic diseases, together with information about the carers of these persons. According to C&SD, the data intends to reflect the situation in 2020. See Census and Statistics Department (2021).
- The data on care recipients discussed in this Essentials refers to care recipients who resided at home (or resided in households). Persons residing in institutions and special classes buildings, meanwhile, are not included.
- Much of the data discussed in the ensuing paragraphs are provided by C&SD upon request by the Research Office.
- Older long-term care recipients are defined as "persons aged 60 and above who currently need relative(s) or other person(s) to take care of their day-to-day living (such as domestic activities, going shopping, going to recreational centre, consulting doctors and taking medicine/receiving treatment) on a long-term basis". See Census and Statistics Department (2023).
- Among these 226 000 older long-term care recipients, 179 000 (i.e. 79%) of them lived together with their primary carers while the remaining 46 000 (21%) were not living together with their primary carers.For the other 95 000 older long-term care recipients (i.e. their primary carers were not their spouses, sons/daughters or sons-in-law/daughters-in-law), around 68 000 and 6 000 had live-in domestic helpers and staff from social welfare organizations as their primary carers respectively; the remnant, around 20 000 care recipients, had other persons (including relatives other than spouses, sons/daughters or sons-in-law/daughters-in-law, and friends) acting as their primary carers.Separately, given primary carers might take care of one or more than one older long-term care recipients, the number of primary carers would likely be lower than the corresponding number of care recipients. Using data from the Thematic Report as an illustration, among cases where the older long-term care recipients lived together with their primary carers, there were 234 000 primary carers responsible for supporting 257 000 older long-term care recipients, i.e. a differential of close to 10%. See Census and Statistics Department (2023).
- Care recipients with disabilities and/or chronic diseases are defined as persons with specific needs (i.e. persons who were encountering difficulty in day-to-day living due to disabilities and chronic diseases, and persons with chronic diseases who were using assistive devices) and had another person taking care of their day-to-day living. For details on definition of persons with disabilities and persons with chronic diseases in the Supplementary Enquiries, see Census and Statistics Department (2021).
- From the Supplementary Enquiries' data provided by C&SD upon request, it can be observed that, in 2020, there were about 36 000 to 69 000 working age care recipients with disabilities and/or chronic diseases receiving day-to-day care from their family/relatives/friends. However, it is difficult to pin-point a more precise figure – there could be duplication between the two sets of data on persons with disabilities and persons with chronic diseases respectively (as a person may suffer from disabilities and chronic diseases at the same time), but ascertaining the degree of duplication is not feasible as the two sets of data were collected from two separate surveys which were conducted over different data collection periods. The figure arising from simply adding the two sets of data directly, therefore, can only be considered an "upper bound" estimate of care recipients.For more detailed data on regarding the caring need and arrangement for persons with disabilities and/or chronic diseases, see Appendix 1.
- Family/relatives include, for example, spouses, parents, children, sons-in-law, daughters-in-law and siblings. Although some commentators consider neighbours as a category of informal carers, this Essentials puts its focus on the roles of family, relatives and friends as carers, thus neighbours are excluded from all data herein.
- The ratios of relevant carers reported to be aged 35-54 and aged 55-64 were 43% and 31% respectively.
- The ratios of relevant carers reported to be aged 35-54 and aged 55-64 were 27% and close to 40% respectively.
- The economically inactive population is made up of those persons who have not had a job and have not been at work during the 7 days before enumeration (excluding persons who have been on leave/holiday during the period and unemployed persons during the 7 days) as well as homemakers, retirees, unpaid carers, persons who are not available for work, and persons who are not seeking work. As for the economically active population (which is synonymous with the labour force), it comprises the employed population and the unemployed population.
- It should be cautioned that the category of unpaid carers depends on self-identification by the respondents. This option, meanwhile, fails to capture carers who are (a) economically inactive and self-identify as other categories such as homemakers, retirees and, for young carers in particular, students; and (b) economically active (i.e. carers participating in the labour market). Besides, the data cannot distinguish the intensity of caregiving responsibilities of carers. While some are heavily involved in caring for day-to-day living of another person (e.g. they act as the primary carers), there are other carers who only provide ad hoc and less intensive caregiving. Hence, the data covers both sole/primary carers and persons with other caregiving responsibilities, and therefore cannot be compared directly with the data on carers obtained from the Supplementary Enquiries and that on carers of older persons from the 2021 Population Census.
- The figure does not include live-in domestic helpers, staff of social welfare organizations (e.g. day care centre services, home-based care services) and "others" (relatives other than spouses, sons/daughters or sons-in-law/daughters-in-law, and friends etc.). The Thematic Report pointed out that when including all formal carers (live-in domestic helpers and staff of social welfare organizations etc.) and informal carers (spouses, sons/daughters, sons-in-law/daughters-in-law, other relatives, and friends), about 29% of primary carers who lived in the same accommodation with their older long-term care recipients were aged 60 and above themselves.
- Elderly unpaid carers are excluded.
- As some unpaid carers might have been responsible for caring for persons residing in another household, the share of elderly persons in unpaid carers in these households is only for reference.
- Another noteworthy observation is that for households with both economically inactive elderly persons and children, elderly unpaid carers accounted for a significantly lesser share of just 6% (800 persons) of the 12 800 unpaid carers in these households, whereas female aged between 35 and 54 years old made up a much more noticeable share of unpaid carers in these households, at 56% (7 100).In fact, among over 160 000 persons who identified themselves as unpaid carers in the 2021 Population Census, the biggest group, at 56% or 90 800 persons, were actually found in households with caring responsibilities likely confined to taking care of children (i.e. households with children but no persons who are economically inactive elderly persons or are working age persons who are economically inactive due to sickness/injury/disablement).
- Earlier, the Government released a consultancy report, mentioning the situations of carers of elderly persons and persons with disabilities. However, the no concrete definition on carers was put forward. See PolyU Consultancy and Technology Co Ltd (2022).
- In relation to a systematic "professional carer system" comprising a tripartite partnership among the Government, professional care providers and carers, it is proposed that professional care providers adopt a case management model to assess the needs for care and attention of the care recipients, enter into a service agreement with the carers to regulate their obligations, and at the same time, provide them with training on proper caring skills. Once a service agreement has been entered into, it is like being accredited by the Government as the carers' social status has been established. See Legislative Council Secretariat (2022).
- To facilitate the public's checking of the vacancies of residential respite places which suit their needs, the Social Welfare Department ("SWD") launched the online "Vacancy Enquiry System for Residential Respite Service for Persons with Disabilities, Residential Respite Service for the Elderly and Emergency Placement for the Elderly" in 2019. SWD plans to enhance the Enquiry System in mid-2023 to cover day respite services, and assist carers' simultaneous search for day and residential respite services through the System. See GovHK (2022c).
- There are criticisms that the threshold is not low for a chronically ill patient to be considered as severely disabled within the meaning of the Social Security Allowance Scheme. Specifically, the applicant must be certified by the Director of Health or the Chief Executive, Hospital Authority (or under exceptional circumstances by a registered medical practitioner of a private hospital) as falling into one of the following categories: (a) illness resulting in being bedridden; (b) a degree of disablement resulting in the applicant needing substantial help from others to cope with daily life (i.e. significant restriction or lack of ability or volition to perform at least one or more of the following activities in daily living to the extent that substantial help from others is required: (i) working in the original occupation and performing any other kind of work for which he/she is suited; (ii) coping with self-care and personal hygiene such as feeding, dressing, grooming, toileting and/or bathing; (iii) maintaining one's posture and dynamic balance while standing or sitting, for daily activities, managing indoor transfer (bed/chair, floor/chair, toilet transfer), travelling to clinic, school, place of work; or (iv) expressing oneself, communicating and interacting with others, maintaining cognitive abilities (orientation, attention, concentration, memory, judgment, thinking, learning ability, etc.), maintaining emotional control and social behaviour). See 1823.gov.hk (2021).
- The 11 recommendations are:
Gear I: Carer Strength Building(a)Raise awareness of carers about the importance, availability, and access of information and increase the readiness of carers and intermediate parties to seek help from available services;(b)Examine existing websites and encourage non-governmental organizations/social enterprises/corporates to develop a carer-centric and sustainable information gateway to address carers' needs;(c)Provide carer-centric training and intervention to promote carers' wellbeing, self management, ability to cope with stress, as well as to strengthen their caregiving capacity;Gear II: Encouraging Family and Informal Support(d)Promote family-based support and mutual assistance among peer carers across their lifespan and at different stages of their caregiving journey;(e)Cultivate a carer-friendly neighbourhood;(f)Devise and promote a carer-friendly support environment in the workplace so as to help carers strike a balance between their work and their caregiving role;Gear III: Service Integration(g)Develop a local self-administered assessment tool with the aim of increasing the knowledge of carers in terms of needs, risks identification and management, and potential support available;(h)Identify high-risk carers and provide timely support;(i)Better introduce, access and utilize assistive technologies to relieve care burden, enhance caring capability and improve carers' quality of life;(j)Increase accessibility and diversity of respite service to provide relief to carers with ad-hoc needs; and(k)Provide good mix of services, voucher and cash to support carers.See PolyU Consultancy and Technology Co Ltd (2022).
- A literature review (covering publications including those from the Organisation for Economic Cooperation and Development ("OECD") and International Alliance of Carer Organizations) indicates that only a handful of advanced places, including Australia, England and the United States, have established both national legislations to provide a legal definition of informal carers as well as systems to formally assess carers' needs. Considering the experience provided by Australia's measures such as Carer Gateway and Integrated Carer Support Service in how to better support carers through multiple channels and personalized action plans, this Essentials chose Australia for more in-depth investigation regarding support measures for carers.For a broad overview of the global landscape regarding support policies for informal carers, a working paper published by OECD in April 2022, though it mainly covers supports to carers of older people, can be of reference value. Overall speaking, the paper noted that:(a)The first line of support for older people is family and friends who provide unpaid non-professional care, often referred to as informal carers. About 60% of older people receiving care report receiving only informal care on average across OECD member states;(b)Legal definitions and assessments of informal carers remain uncommon: 20% of European Union member states and Australia have a legal definition of informal carers (though more countries have taken steps to recognize them). While most legal/ad-hoc definitions focus on the close bond to the person in need of care, criteria to target carers for support measures often involved the type of relationship, co residency, the type of care provided and the number of hours of care;(c)About two-thirds of the 33 studied OECD member states provide cash benefits to informal carers – these are either paid directly to carers through a carer allowance (61% of member states), or paid to those in need of care, at least part of which is in turn used to compensate formally registered family carers (39% of member states);(d)Over the past decade, OECD member states have taken steps to facilitate access to information - mostly with digital tools;(e)OECD member states mostly rely on the voluntary sector for training and counselling;(f)Respite care (vast majority provided via in-kind format) remains insufficient and has low uptake (due to low compensation, low availability of services and organizational challenges); and(g)There is growing commitment to support informal carers who combine work and care: Nearly two-thirds of member states provide some rights to leave to care for a family member (either paid or unpaid); about half of them offer some form of paid leave for caring, which tends to be restricted to a shorter duration; however, flexible work-arrangements specific to carers remain uncommon given that over half of employees across OECD member states have their working hours strictly set by their companies.See Organisation for Economic Cooperation and Development (2022).
- In May 2009, Australian House of Representatives Family, Community, Housing and Youth Committee published a report entitled "Who Cares ...?". Apart from urging for "immediate financial relief" for carers, the report also advocated for greater access to respite services (as a "time-out" for carers from their caring roles), better coordination of support services, setting up a one-stop shop for information on community care services, establishing nationally consistent and streamlined support systems, promulgating a national carer recognition legislation, and improving training and support to carers in employment. See Standing Committee on Family, Community, Housing and Youth, House of Representatives (2009a, 2009b).
- Each of the six states and two territories in Australia have carer laws and/or policies. See Carer Gateway (undated).
- The relevant figure was 11.6% in 2015. See Australian Bureau of Statistics (2019).
- Defined as having any limitation, restriction or impairment which restricts everyday activities and has lasted, or is likely to last, for at least six months. See Australian Bureau of Statistics (2019).
- Of people receiving the Carer Payment at September 2022, 80% were being paid the full rate of payment (meaning their assets and income were both below relevant thresholds) and almost half (49%) had been receiving the payment for 5 years or more. See Australian Government (2022).
- See Department of Social Services (2022b).
- See Australian Institute of Health and Welfare (2021a).
- See Department of Social Services (2022b).
- A$2.8 million (HK$15 million) was allocated for 2022-23. See Department of Social Services (2022b).
- The programme was introduced in 2020 as a 3-year pilot scheme, though Internet search indicates that the programme is still on-going with applications accepted during July to September each year. The Department of Social Services requires all successful Young Carer Bursary applicants to complete a mandatory survey in May and October each year to assess their ongoing eligibility. Recipients will be considered ineligible if they are no longer studying (including deference and leave of absence), receive another bursary or scholarship, do not complete surveys and/or have ended their caring roles. Recipients will receive A$2,000 (HK$11,000) at the start of the year, and then receive a second payment of A$1,000 (HK$5,500) in June after completing the mid-year survey in May. They can use the funding towards education or training, including but not limited to school fees, laptops and software, uniforms, transport and accommodation, respite care, emotional support, and extracurricular activities. See Department of Social Services (2020) and Young Carer Network (undated-a, undated-b, undated-c).
- See Department of Social Services (2018).
- One exception would be when carers request for emergency respite care. In such case "emergency procedures" will be triggered immediately and emergency respite services will be secured for the carers first. Carers support planning will be undertaken in follow up contacts. For carers who access services online, they could request a call-back by Regional Delivery Partners ("RDP") or get referred to RDP to follow the Carer Support Planning Process, in addition to browsing the information on the Carer Gateway website and determining the most appropriate resources on their own. See Department of Social Services (2018).
- Subsidies depend on the level of care provided in the Home Care Packages ("HCP"). Supplemental subsidies may also be made available if certain criteria are met (dementia cases, Veterans, living in rural and remote areas etc.) and/or additional services are required (e.g. oxygen and enteral feeding).
- At 31 December 2022, around 573 300 people were active participants in the National Disability Insurance Scheme ("NDIS"). The top 5 groups, by primary disability, were autism (35% or around 199 400 people), intellectual disability (17%/98 800), psychosocial disability (10%/59 500), developmental delay (10%/56 800) and hearing impairment (4%/25 600); in terms of age profile, 51% (around 290 200 people) were aged 18 or under, 25% (142 100) were aged 19-44, and 25% (141 000) were aged 45 and above (it is noted that aged 65 and above beneficiaries accounted for 4%). See National Disability Insurance Agency (2022).
- Budget for the NDIS in 2022-23 amounted to A$24.1 billion (HK$130 billion). See Department of Social Services (2022b).
- Other categories include consumables, assistive technology, coordination of supports, improved living arrangements, increased social and community participation, finding and keeping a job, improved relationships, improved health and wellbeing, improved learning, improved life choices and improved daily living.
- Examples include (a) the Information, Linkages and Capacity Building program which provides funding to deliver community projects that benefit all people with disabilities, their carers and families; and (b) Community Mental Health programs that provide assistance to people with mental illness and their families and carers to manage the impacts of mental illness on their lives and improve their overall wellbeing.
- See Australian Institute of Health and Welfare (2021a).
- Respite services account for a small component of the Commonwealth Home Support Programme ("CHSP"). The Programme is an entry-level home support program that helps older people to live independently in their homes and communities, with an aim to help people live as independently as possible through a small amount of help. Most people in the CHSP only need one or two services from the programme. See Department of Health and Aged Care (2022a).
- Representing 25% of all respite admissions; nevertheless, it should be noted that not all family members are informal carers.
- For reference: there were 275 600 elderly persons with disabilities; among them, 87 900 reported residing in homes and having family/relatives/friends as their sole or primary carers to take care of their day-to-day living.
Essentials are compiled for Members and Committees of the Legislative Council. They are not legal or other professional advice and shall not be relied on as such. Essentials are subject to copyright owned by The Legislative Council Commission (The Commission). The Commission permits accurate reproduction of Essentials for non-commercial use in a manner not adversely affecting the Legislative Council. Please refer to the Disclaimer and Copyright Notice on the Legislative Council website at www.legco.gov.hk for details. The paper number of this issue of Essentials is ISE02/2023.